The Imperative of Smarter Clinical Information Systems
How AI agents and openEHR Can Lift Healthcare Out of Its Purgatory
TL;DR - Hospitals don’t need more bolt‑on AI dashboards; they need to stop spending human hours transcribing voice notes, scanned referrals, and faxes into databases. Multimodal AI can now structure any input, and openEHR turns that structure into lasting, shareable knowledge. The combo wipes out form fatigue, bridges wildly different local workflows, and fades into the background so clinicians can get back to medicine.
A Perfect Storm of Cost, Complexity & Burnout
Across the globe, healthcare is wrestling with more than flashy new tech - it’s staring down an economic crunch that hits clinicians right where it hurts: time. Administrative chores siphon off billions, drive burnout to record highs, and threaten the financial breathability of hospitals.
I watch it daily. As Lead of AI Engineering at Cistec AG - makers of KISIM, Switzerland’s leading CIS (Clinical Information System) - we see flashy pilots developed elsewhere stall because they bolt beside existing workflows instead of inside them: another login, another window, more juggling for doctors and nurses already juggling too many.
It’s time for a CIS revolution. Fuse mature, multimodal, agentic AI with openEHR’s clinician‑curated data models and the intelligence disappears into the flow. Notes dictate themselves, documents self‑organize, forms pre‑fill - backed by structured, clinically validated data you can trust.
Crack the admin problem first and you unlock capacity, morale, and cash for everything else.
Administrative Burden → Economic Time‑Bomb
Swiss healthcare’s admin bill isn’t just a line item; it’s ballast. The numbers and ward‑floor stories say it all:
Physicians: 114 min/day on documentation (≈ 20 % of their shift); 67 % report patient‑safety slips after late‑night report‑writing.
Nurses: 74 % feel “heavily burdened” by paperwork; 1 in 3 logs ≥ 2 h admin per shift. About a third screen positive for burnout.
Residents: 56‑hour weeks; half admit they “can’t go on.”
Hospitals pay in cash, too: a federal audit pegs 16–19 % of spending as avoidable waste - mostly duplicated data entry and information chasing.
🌍 And this isn’t just Switzerland. The same documentation purgatory spans every corner that practices modern medicine.
Absurd 2025 scene: junior doctors act as digital scribes, copy‑pasting diagnoses and medication lists from old PDFs or referrals, then re‑prescribing every drug one field at a time. Clinical value added: zero. Human frustration: max.
Why “Fix It Later” Is No Longer an Option
Every day we stall, that paperwork drag converts directly into overtime invoices, locum fees, and missed‑revenue leaks. Solving it isn’t about shaving ten seconds off a dialog box; it’s about rewiring how data is captured and reused.
When all information is structured once and reused everywhere, four levers move together:
1. 🩺 Free Capacity, Cut Burnout
Automation lifts the slog of dictations, PDFs, and faxes, handing back hours for patient care and trimming locum spend.
2. 💼 Super‑charge Operational Intelligence
openEHR‑clean data turns bed, theatre, and staffing planning into data science, not educated guesswork.
3. 🔧 Build Longitudinal Gold
Notes, vitals, and labs stack into lifelong patient timelines - fuel for today’s quality metrics and tomorrow’s precision medicine.
4. 💸 Slash Error Loops & Hidden Costs
Capture data right the first time and you eliminate claim denials, audit rework, and those “please re‑send” calls all while averting safety events born of missing info.
Pan‑European studies peg the upside in the multi‑billion‑franc range, and Switzerland’s own 2023 digital‑transformation program calls for exactly this structure‑first playbook.
Bottom line: the human toll makes action urgent; the economic math makes delay indefensible. Time to break the paperwork ballast and let hospitals breathe.
The Tech That Makes "Invisible Intelligence" Work: openEHR + AI Agents
So, how do we build a CIS that actually reduces friction and disappears into the workflow? It takes two core components working in tight synchrony: the rock-solid, clinically validated data structures of openEHR, and the flexible, context-aware processing power of multimodal AI agents. Forget bolt-on dashboards; this is about embedding intelligence from the ground up.
openEHR: The Bedrock for Trustworthy, Adaptable Systems
If AI is the muscle, openEHR is the skeleton that keeps it aligned and safe. Hospitals aren't adopting this open standard for fun; they're choosing it because nothing else reliably converts messy clinical reality into computable, shareable, future-proof knowledge while keeping clinicians in control. Here’s the crucial difference it makes:
Clinician-Driven Structure & Guardrails: Every data point maps to models (archetypes & templates) drafted and validated by clinical experts. These define not just the data type (e.g., temperature) but also crucial constraints – allowed units (°C only), plausible value ranges (no 400°C fevers!), required terminology codes. These rules act as built-in safety checks for any input, human or AI.
Semantic Interoperability Baked In: A blood pressure reading captured using the standard archetype means the exact same thing clinically, whether entered in Basel or Geneva. This inherent shared meaning smashes data silos and aligns perfectly with Switzerland’s national interoperability goals.
Vendor Neutrality & Adaptability: The open specification means hospitals own their data structures. Need to add a field to the endocrine follow-up? Clinicians update the template; the AI agents adapt instantly. Swapping out an application layer doesn't require a painful data migration. This avoids vendor lock-in and keeps the system clinically relevant over time.
Built-in Validation & Audit: Those clinical constraints are automatically checked on every save. Every change is versioned and attributed. No more compliance and governance headaches.
Bottom line: openEHR provides the essential trust layer. It ensures that the "invisible" AI operates within safe, clinically agreed-upon boundaries.
Multimodal & Agentic AI: The Engine That Erases Workflow Friction
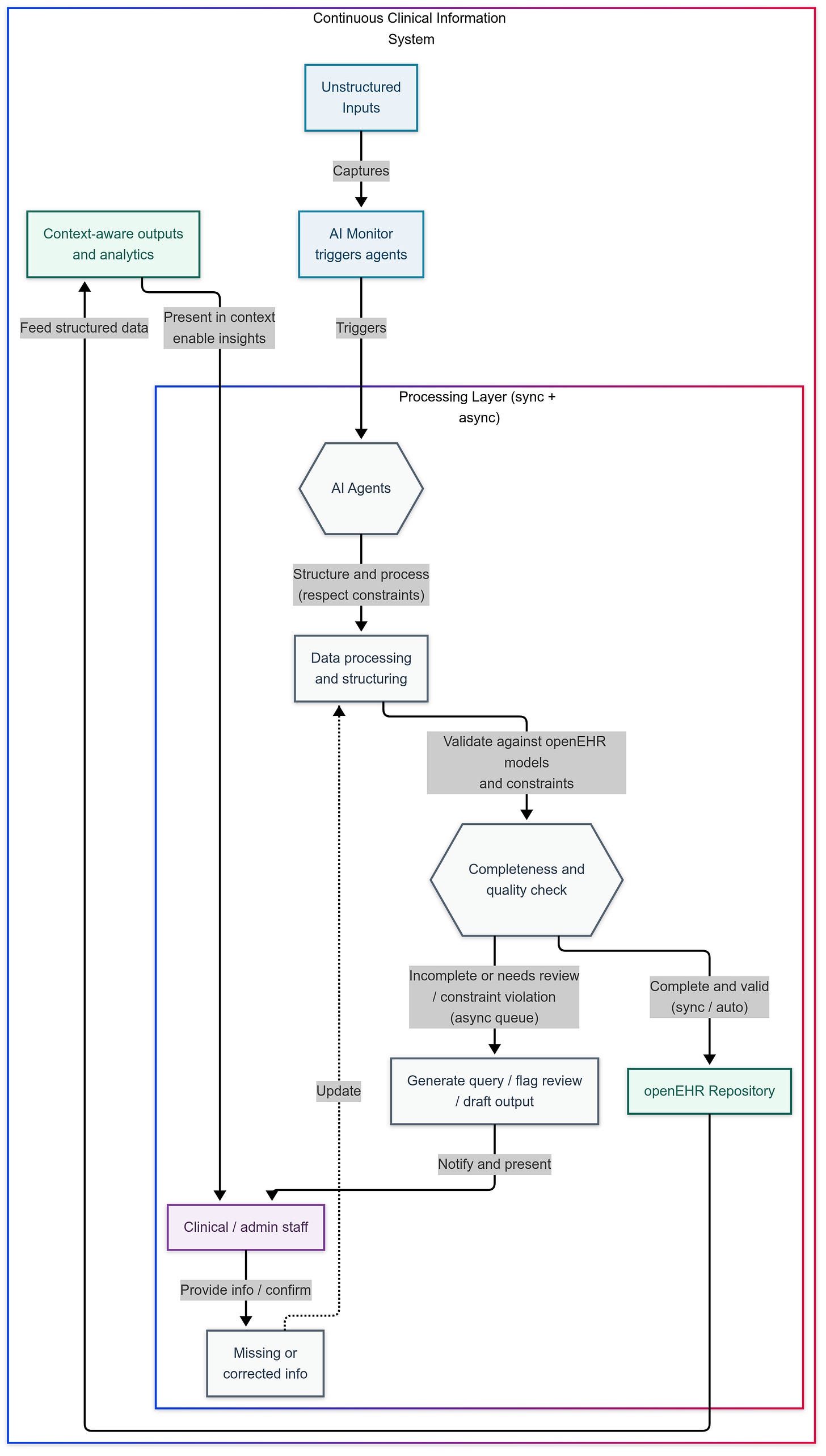
If openEHR defines the trustworthy "what" of the data, AI agents handle the "how" – processing information and automating tasks with minimal friction. They understand context, handle diverse inputs, and interact naturally, always respecting the openEHR guardrails:
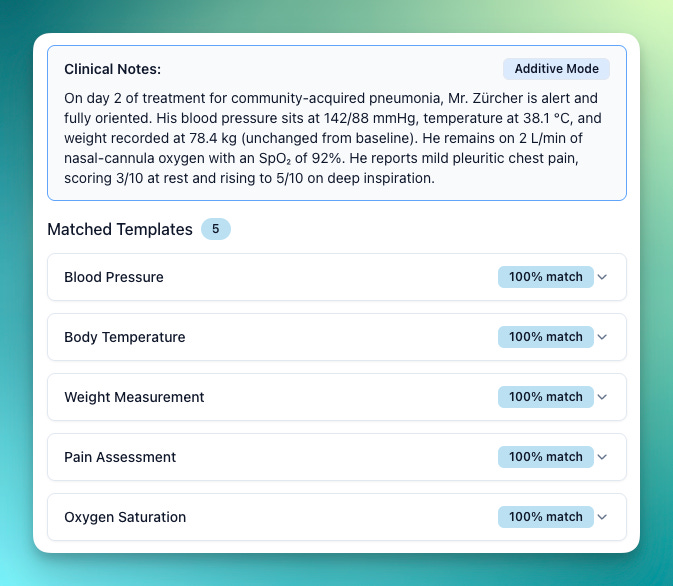
Universal Input Processing: Forget rigid forms as the only gateway. AI agents act as universal translators, ingesting information from any source – voice dictation, ambient conversation ("hallway chat"), scanned referral PDFs, faxes, structured forms, FHIR, even sensor data – and structuring it into pristine openEHR records behind the scenes. This eliminates the soul-numbing "digital scribe" work.
Natural Interaction & Context Awareness: Interact via voice or text directly within your workflow. The agent parses intent, pre-fills relevant data based on context (e.g., knowing you're on a ward round vs. in billing), and only prompts for clarification when necessary. Help appears where you are, when you need it, then gets out of the way.
Embedded Task Automation (Sync & Async): This is key – moving beyond just displaying information to doing work. Fueled by reliable openEHR data, agents can:
Instantly validate vitals or simple observations (synchronous).
Automatically pre-fill discharge summaries or suggest medical codes based on the narrative, queueing them for quick human review if needed (asynchronous).
Proactively trigger downstream actions like placing standard orders or sending referral notifications upon data validation.
Stitch context by automatically linking related labs, notes, meds, and problems for a holistic view.
Intelligent Output & Summarization: Information is presented contextually where needed – brief summaries embedded in workflows, adaptive views showing only relevant data points, answers to natural language queries appearing without switching screens. Generative UI can even build temporary forms and charts on the fly based on the immediate need.
Tuesday 07:03 - Dictation captured ambiently, key vitals automatically extracted and validated, AI flags a potential medication interaction for human review based on the structured record, initiates a query for a rehab bed based on documented goals, and drafts the handover note incorporating all validated data. Zero extra clicks, zero context switches.
Illustrative Applications: Harnessing Structured Data
Once your information sits as clean, trustworthy openEHR records, admin efficiency is just the opening act. That foundation unlocks a stack of high‑value moves with almost no extra lift:
💸 Super‑charged coding & billing
Agents mine the structured narrative, surface1 / CHOP2 / TARMED3 codes, and flag the quirky edge cases for a two‑second human sweep - slashing manual effort and boosting revenue integrity.
🏥 Clinically‑aware resource insights
With patient acuity, diagnoses, and interventions all computable, the AI can forecast bed demand, spot discharge bottlenecks, and optimize patient flow based on real clinical drivers - not gut feel.
🛡️ Streamlined authorizations & compliance
Need prior approval? The agent bundles the exact clinical rationale straight from the record, checks it against quality measures, and flags gaps before auditors - or insurers - do.
📊 Effortless reporting
Quality metrics, admin KPIs, registry feeds, all generated automatically from the validated data store. Accurate, consistent, and on time, minus the spreadsheet heroics.
🔬 Powerful cross‑patient insights
Want every patient with a tricky comorbidity pattern? Or outcomes across a demographic slice? Longitudinal, structured data makes complex queries routine, driving better care pathways and sharper population‑health research.
Structure the data once, and the payoff keeps compounding.
Navigating Implementation: People, Process & Integration
Technology is only half the battle; success hinges on thoughtful rollout and human factors:
🩺 Workflow‑first design. Every new feature must lose clicks, not add them. If a prototype creates friction, back to the drawing board.
🔧 Integration reality‑checks. Legacy HL74 feeds, home‑grown middleware, decade‑old scanners - they’re not vanishing overnight. Pragmatic interfacing and staged cut‑overs keep the lights on while you modernize.
💼 Change management. Clear comms, targeted training, and quick visible wins turn skeptics into champions. Tech never adopts itself.
🩺 🔧 Reskilling the workforce. With agents taking over routine work, clinicians move into oversight and analysis roles. That shift demands coaching, not wishful thinking.
Guardrails: Proving the Invisible Layer Plays by the Rules
Building trust in this 'invisible' layer is paramount. That requires clear guardrails:
Explainability everywhere: every agent logs inputs, model version, fired rules, confidence. One‑click provenance.
Human veto: low‑confidence items park in an async queue until a clinician taps accept / tweak / reject.
The Path Forward
Let's be clear: this isn't vaporware. My team and I at CISTEC are already actively researching and building this vision today at the same time as introducing immediate high-impact AI features on top of our existing platform.
This is however, still a journey and not a finished product. I’ll be sharing the real story – progress, hurdles, and demos – at the 2nd openEHR.ch Symposium on May 5th, 2025. Hope to see you there.
What’s Next on This Substack: Follow for the Deep Dives
Skip the hype cycle and get the engineering trenches view. Hit Subscribe and you’ll see:
Beyond openEHR: How do we deal with data that isn’t stored in openEHR.
UX / Generative UI: “Agent inboxes”, human-in-the-loop patterns, forms that build themselves so clinicians never click twice.
Ask‑the‑Data: plain‑language SQL vs AQL5 and everything in between.
Agent Ops: orchestration patterns, guardrails and chaos‑prevention for multi‑agent fleets.
Reality Checks: Use-case specific LLM benchmarks, on‑prem OSS, privacy strategies that pass audit.
Change & Compliance: EU AI Act cheat‑sheet, MDR, Swiss data law, war stories from roll‑outs.
Design for Everyone: voice‑first, multilingual, and accessibility that actually works.
👉 Subscribe for the Deep Dives
Hit Subscribe to get every future instalment delivered straight to your inbox. Have a burning question you want me to tackle? Just hit reply and let me know—I’ll work it into a coming post.
🎉 20% Off Forever
To celebrate finally shipping this brainwave, I’m offering a 20 % lifetime discount on all subscriptions—lock it in before 31 May 2025!
Conclusion
Alright, let's land this plane. The takeaway? Healthcare isn't just inefficient; it's actively hostile to clinicians' time and focus thanks to clunky systems and that soul-crushing "workflow tax." Just creating poorly integrated AI dashboards isn’t the answer.
The real fix starts deeper: using AI agents to intelligently structure every piece of information – voice notes, scanned docs, sensor streams – and locking it down reliably with openEHR's clinician-defined rules. That combo gives you data you can trust and intelligence that works for you, one that disappears into the workflow.
The system I’ve outlined here slashes avoidable costs, turbo‑charges decision‑making, and lifts care quality - all while handing clinicians the gift of time. The tech is ready, the ROI is on the table, and the need is impossible to ignore. Let’s replace today’s documentation sinkhole with systems that let doctors and nurses spend their time on medicine - not paperwork.
ICD - International Classification of Diseases (diagnosis codes)
CHOP - Swiss Classification of Surgical Procedures (CH‑OP)
TARMED - Swiss outpatient medical tariff system
HL7 - Health Level Seven (health‑data messaging standard)
AQL - Archetype Query Language (openEHR query syntax)





Really insightful. I really like the emphasis on embedding intelligence into a workflow instead of making it complicated by adding extra clicks. In the end, the goal is to save time and increase adoption, not to overcomplicate things. Looking forward to seeing this happen.
Great article and insights 🙌 Looking forward to seeing it become reality at Cistec.